The peritoneum covers the abdominal wall and the viscera. The malignant tumors that originate from organs of the abdominal cavity have the property to spread at the peritoneal surfaces in approximately 50%. This results to peritoneal malignancy.
The peritoneal malignancy that originates from an epithelial cancer is called peritoneal carcinomatosis. If it originates from a sarcoma it is called peritoneal sarcomatosis. The term that has been generally accepted in Greek terminology for peritoneal malignancy is generalized abdominal carcinomatosis.
Until recently peritoneal malignancy had been considered surgically irresectable and systemic intravenous chemotherapy had been used for palliation. The most frequent disease with peritoneal dissemination is ovarian cancer. In ovarian cancer patients, surgical resection of the tumor load has been shown to increase survival. The same results have been demonstrated in appendiceal cancer. The same surgical technique was used in patients with colorectal cancer or gastric cancer. Surgical resection was shown to offer survival benefit compared to conservative treatment with intravenous chemotherapy alone. In addition, surgical resection of peritoneal mesothelioma has been shown to be superior over conservative treatment.
The resection of peritoneal malignancy is possible with cytoreductive surgery. The purpose of cytoreductive surgery is the maximal resection of the tumor load. The residual tumor must not be macroscopically visible if possible. This is not always possible, particularly if the small bowel has been seeded. The resection of the entire small bowel is not compatible with life because the absorption of energy fuel is not possible. In case that the small bowel has not been entirely seeded and the healthy residual one is capable of absorbing the required fuel depots then the possibility of complete resection of the tumor increases.
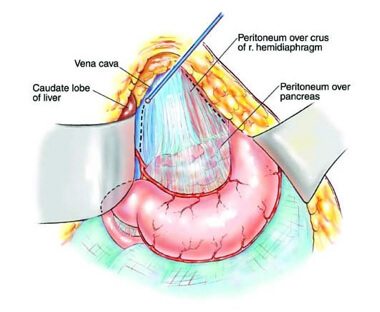
Cytoreductive surgery is possible with standard peritonectomy procedures as have been described by P. H. Sugarbaker, inventor of cytoreductive surgery in surgical oncology. Complete or near complete cytoreduction is possible only by using standard peritonectomy procedures. As a consequence, surgery is the most powerful tool in peritoneal malignancy treatment. There is one question left. What happens to the microscopic or the very small visible tumor that is left behind after surgery?
The answer has been given from Washington Hospital Center, by P. H. Sugarbaker by both clinical and experimental data. The results of surgery in which intraperitoneal chemotherapy is integrated are extraordinary.
Most of the cytostatic drugs that are given in the abdominal cavity are macromolecular substances that have the property to act for long at the peritoneal surfaces. This results in the eradication of the microscopic tumor that is smaller than 2-3mm at its largest diameter. The penetration and action of cytostatic drugs in tumors with largest diameter is not possible.
This treatment is ideal for pseudomyxoma peritonei, appendiceal cancer, colorectal cancer, ovarian cancer, peritoneal mesothelioma, gastric cancer, cancer of the small bowel, and peritoneal sarcomatosis.
Intraperitoneal chemotherapy is also used for those patients that are in high risk to develop peritoneal malignancy. Intraperitoneal chemotherapy may be used in locally advanced tumors of the stomach, colon, rectum, small bowel, ovaries, pancreas, corpus uteri, or vagina with the intention to stop the development of tumors that will grow in 2-3 years after initial surgery.
Intraperitoneal chemotherapy may be used either during surgery combined with high temperature ((42-42.50C) or after surgery during the first 5 postoperative days under normothermia before the presence of adhesions.
This type of chemotherapy has many advantages and minimal side effects because it is given only once and is absorbed slowly in the systemic circulation.